Άμεση Εξυπηρέτηση Επειγόντων - Ερευνητικά Τεκμηριωμένες Παρεμβάσεις
Τι λένε οι ασθενείς... Διαβάστε περισσότερα
Αθανασία Α.
Ο κύριος Δανάλης είναι πολύ σωστός επαγγελματίας δίνει την απαραίτητη προσοχή στον ασθενή και στο πρόβλημα που έχει.Το πιο σημαντικό όμως είναι η ποιότητα και αποτελεσματικότητα της θεραπείας, με τρόπο δημιουργικό και κυρίως αποδοτικό. Τον προτείνω ανεπιφύλακτα.
Εριφύλη Σ.
Ο κος Δανάλης γνωρίζει πολύ καλά το αντικείμενό του και ασχολείται προσωπικά και πολύ με τον ασθενή του! Έχει θετική διάθεση και με έχει βοηθήσει πολύ!! Του έχω πολύ εμπιστοσύνη και τον συστήνω ανεπιφύλακτα.
Γιώτα Σ.
Γνωρίζει πολύ καλά το αντικείμενο του, και ασχολήθηκε πολύ ώρα με το πρόβλημα μου και πραγματικά κέρδισε την εμπιστοσύνη μου! Θα τον συστήσω σίγουρα!
Κλείστε Ραντεβού

Κωνσταντίνος Δανάλης, PT
Φυσικοθεραπευτής
Αδειούχος Φυσικοθεραπευτής μέλος του Πανελλήνιου Συλλόγου Φυσικοθεραπευτών και μέλος στα εξειδικευμένα τμήματα του Συλλόγου:
Επιστημονικό Τμήμα Μυοσκελετικής Φυσικοθεραπείας
Επιστημονικό Τμήμα Θεραπευτικής Άσκησης
Επιστημονικό Τμήμα Φυσικοθεραπείας για την Ψυχική Υγεία
Aπόφοιτος του Πανεπιστημίου Δυτικής Αττικής
Ειδικός σε:
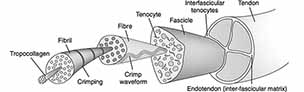
Μυοσκελετικά προβλήματα και παθήσεις
Διαχείριση Σπονδυλικής Στήλης - Αυχεναλγίες, Οσφυαλγίες
Μυοσκελετικές κακώσεις λόγω τραυματισμού ή υπέρχρησης
Εξειδικευμένη αντιμετώπιση λανθασμένων κινητικών προτύπων, νευρομυϊκού συντονισμού και άλλων αιτιών που έχουν σημαντικό αντίκτυπο στην καθημερινότητα του ασθενή, την κινητικότητα και τη λειτουργικότητά του, εν τέλει στην ποιότητα ζωής του.
Εφαρμόζει τις πιο σύγχρονες, επιστημονικά αποδεδειγμένες τεχνικές και θεραπείες για μυοσκελετικές παθήσεις, ανακούφιση του πόνου, και βελτίωση της λειτουργικότητας και της ποιότητας ζωής του ασθενή.